Understanding Varicose Veins: Causes and Symptoms
- deepikavedyan
- Jul 28
- 5 min read
Varicose veins are often seen as a cosmetic issue, but the truth is far more complex. These swollen, twisted veins, most commonly found in the legs, may signal underlying circulatory problems that can lead to serious health complications if ignored. While some people may experience only minor discomfort, others face pain, skin changes, and an increased risk of blood clots.
This article explores what causes varicose veins, the symptoms you should pay attention to, the risks of leaving them untreated, and when it is time to consult a specialist. Understanding this condition can help you take informed action toward better vascular health.
What Are Varicose Veins and Why Do They Occur?
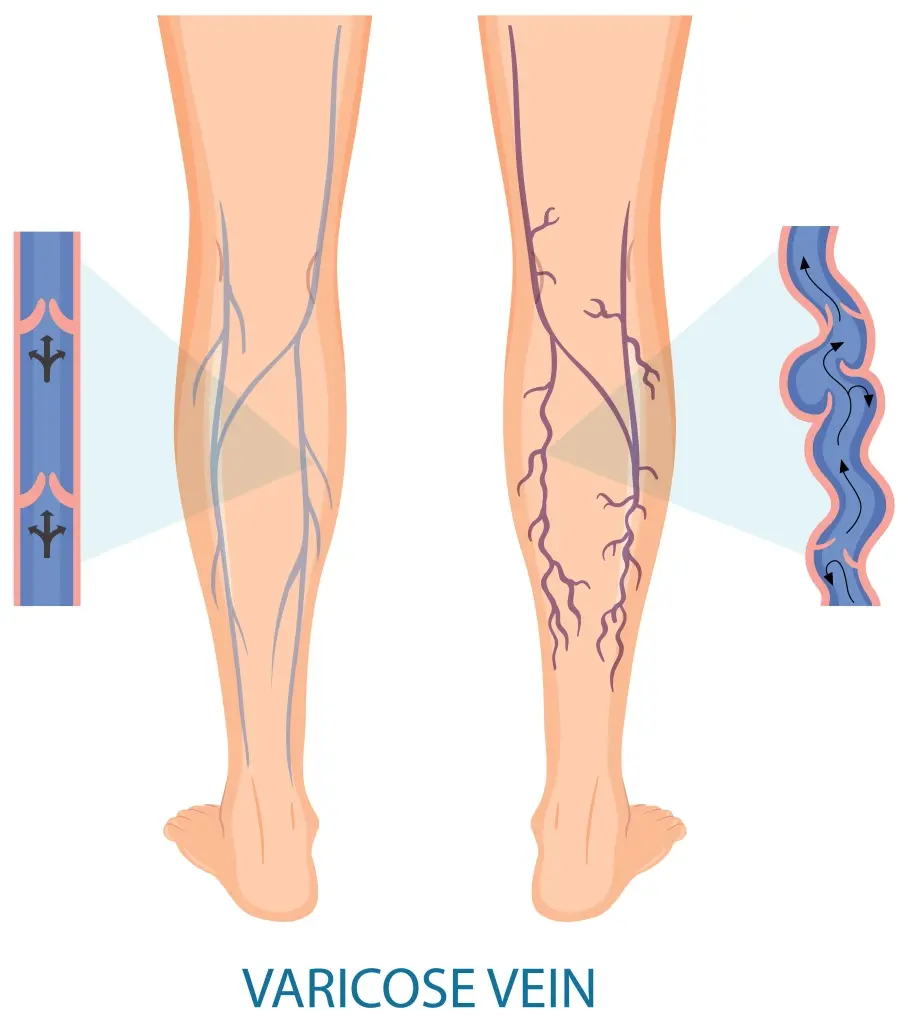
Varicose veins develop when the one-way valves in the veins become weak or damaged, causing blood to pool instead of flowing smoothly back to the heart. As a result, veins become enlarged, twisted, and visible beneath the skin. This condition most commonly affects the legs and feet due to the increased pressure exerted when standing or walking.
Several factors contribute to the development of varicose veins. According to Dr Manish Rajput, one of the most significant is genetics. If your parents or grandparents had varicose veins, your risk is notably higher. Age is another major factor. As we grow older, veins lose elasticity and the valves may not work as efficiently, increasing the likelihood of blood pooling.
Hormonal changes, particularly in women during pregnancy, menstruation, or menopause, can also affect vein health. These changes relax vein walls and contribute to the development of varicose veins. Occupations that require prolonged standing or sitting, such as nursing, teaching, or working at a desk, can further elevate the risk.
Obesity, sedentary lifestyles, and smoking are additional risk factors. When the veins are under more pressure than they can handle, the valves are more likely to fail, resulting in varicose veins.
Common Symptoms You Shouldn’t Overlook
While varicose veins are often easily recognized by their bulging, bluish appearance just beneath the skin, the physical signs are only part of the story. Symptoms can range from mild to severe and may affect quality of life if not addressed early.
One of the first signs many people notice is a feeling of heaviness or aching in the legs, especially after standing for extended periods. This discomfort usually worsens toward the end of the day and may improve with leg elevation or rest. Cramping, burning, or throbbing sensations are also common complaints.
Swelling in the lower legs and ankles is another warning sign. Over time, skin around the affected veins may become dry, itchy, or discolored. In more advanced cases, the skin can harden and ulcers may form near the ankles, which are difficult to heal and prone to infection.
Restless legs, particularly at night, may also be linked to underlying venous disease. If you find yourself needing to move your legs constantly or are awakened by leg discomfort, it may not be just fatigue or dehydration. It could be a symptom of venous insufficiency.
Importantly, symptoms do not always correlate with the visual appearance of the veins. Some individuals with small or minimal visible veins may experience significant discomfort, while others with prominent varicose veins might report few symptoms. Regardless of appearance, persistent leg pain, swelling, or changes in skin texture warrant medical evaluation.
Potential Health Risks of Untreated Varicose Veins
Ignoring varicose veins can lead to more than just aesthetic concerns. Left untreated, they can result in a range of complications, some of which are potentially serious and even life-threatening.
One of the most common complications is chronic venous insufficiency, a condition where blood flow through the veins becomes severely impaired. Over time, this can lead to long-term swelling, skin thickening, and venous ulcers. These ulcers are painful and difficult to manage, especially in older adults or individuals with diabetes.
Another significant risk is superficial thrombophlebitis, where a blood clot forms in a vein near the surface of the skin. While it may sound less serious than deep vein thrombosis (DVT), it can cause localized pain, redness, and warmth and may signal broader venous disease.
Perhaps the most dangerous complication is Deep Vein Thrombosis. This occurs when a blood clot forms in a deeper vein, typically in the leg. If the clot breaks loose, it can travel to the lungs and cause a pulmonary embolism, a medical emergency that can be fatal if not treated immediately.
Bleeding is another concern. Varicose veins that are close to the skin surface can rupture, sometimes even from minor trauma. The resulting bleeding can be significant and may require emergency care.
These complications highlight why varicose veins should never be considered a harmless cosmetic issue. Timely diagnosis and treatment can prevent escalation and protect your long-term health.
When to See a Specialist and What to Expect
Knowing when to seek medical help for varicose veins is crucial. If you are experiencing persistent leg pain, swelling, or skin changes, or if your veins are causing discomfort during daily activities, it is time to consult a vascular specialist or a doctor who focuses on vein disorders.
You should also consider a professional evaluation if:
The veins are worsening over time
You notice skin discoloration or ulcers
There is a family history of venous disease or blood clots
Your symptoms interfere with sleep or physical activity
You have experienced bleeding from a vein
During your visit, the specialist will take a detailed medical history and perform a physical examination. In most cases, a duplex ultrasound is used to evaluate blood flow and identify areas of valve dysfunction or clot formation. This non-invasive imaging helps the doctor understand the severity of your condition and plan appropriate treatment.
Fortunately, modern Varicose Vein Treatment options for varicose veins are highly effective and much less invasive than traditional surgery. Many procedures are performed in an outpatient setting and involve minimal recovery time.
Endovenous laser therapy (EVLT) and radiofrequency ablation (RFA) use targeted heat energy to seal off affected veins. Sclerotherapy involves injecting a solution into the vein, causing it to collapse and eventually fade. Microphlebectomy is a minor procedure that removes surface veins through tiny skin punctures.
Lifestyle changes also play an important role. Maintaining a healthy weight, exercising regularly, avoiding long periods of standing or sitting, and wearing compression stockings can help manage symptoms and prevent progression.
Most patients experience relief soon after treatment, and recurrence is less common with modern techniques. Early intervention not only reduces symptoms but also prevents future complications, allowing you to maintain better vascular health and enjoy a more active lifestyle.
Conclusion
Varicose veins are more than just a cosmetic concern. They can signal deeper issues with your circulatory system and lead to serious complications if left untreated. Understanding the causes, recognizing symptoms early, and seeking timely medical advice can make a significant difference in your overall health and well-being.
If you or someone you know is experiencing signs of varicose veins or related vein conditions, do not delay in speaking with a healthcare professional. With advancements in diagnostic tools and treatment options, managing varicose veins is more accessible, effective, and comfortable than ever before.




Comentarios